Which Are The Main Causes Of Adult Aquired Flat Feet ?
Overview Originally known as posterior tibial tendon dysfunction or insufficiency, adult-acquired flatfoot deformity encompasses a wide range of deformities. These deformities vary in location, severity, and rate of progression. Establishing a diagnosis as early as possible is one of the most important factors in treatment. Prompt early, aggressive nonsurgical management is important. A patient in whom such treatment fails should strongly consider surgical correction to avoid worsening of the deformity. In all four stages of deformity, the goal of surgery is to achieve proper alignment and maintain as much flexibility as possible in the foot and ankle complex. However, controversy remains as to how to manage flexible deformities, especially those that are severe. 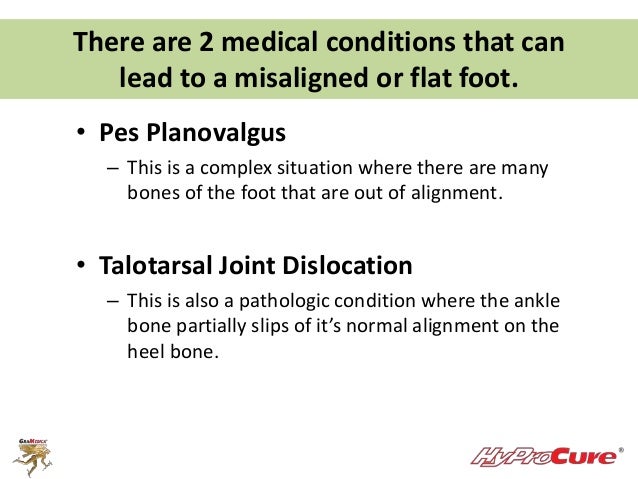 Causes Many health conditions can create a painful flatfoot, an injury to the ligaments in the foot can cause the joints to fall out of alignment. The ligaments support the bones and prevent them from moving. If the ligaments are torn, the foot will become flat and painful. This more commonly occurs in the middle of the foot (Lisfranc injury), but can also occur in the back of the foot. In addition to ligament injuries, fractures and dislocations of the bones in the midfoot can also lead to a flatfoot deformity. Symptoms Your feet tire easily or become painful with prolonged standing. It's difficult to move your heel or midfoot around, or to stand on your toes. Your foot aches, particularly in the heel or arch area, with swelling along the inner side. Pain in your feet reduces your ability to participate in sports. You've been diagnosed with rheumatoid arthritis; about half of all people with rheumatoid arthritis will develop a progressive flatfoot deformity. Diagnosis The diagnosis of tibialis posterior dysfunction is essentially clinical. However, plain radiographs of the foot and ankle are useful for assessing the degree of deformity and to confirm the presence or absence of degenerative changes in the subtalar and ankle articulations. The radiographs are also useful to exclude other causes of an acquired flatfoot deformity. The most useful radiographs are bilateral anteroposterior and lateral radiographs of the foot and a mortise (true anteroposterior) view of the ankle. All radiographs should be done with the patient standing. In most cases we see no role for magnetic resonance imaging or ultrasonography, as the diagnosis can be made clinically. Non surgical Treatment Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In many cases of PTTD, treatment can begin with non-surgical approaches that may include. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe. Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weight-bearing for a while. Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may advise changes to make with your shoes and may provide special inserts designed to improve arch support.
Causes Many health conditions can create a painful flatfoot, an injury to the ligaments in the foot can cause the joints to fall out of alignment. The ligaments support the bones and prevent them from moving. If the ligaments are torn, the foot will become flat and painful. This more commonly occurs in the middle of the foot (Lisfranc injury), but can also occur in the back of the foot. In addition to ligament injuries, fractures and dislocations of the bones in the midfoot can also lead to a flatfoot deformity. Symptoms Your feet tire easily or become painful with prolonged standing. It's difficult to move your heel or midfoot around, or to stand on your toes. Your foot aches, particularly in the heel or arch area, with swelling along the inner side. Pain in your feet reduces your ability to participate in sports. You've been diagnosed with rheumatoid arthritis; about half of all people with rheumatoid arthritis will develop a progressive flatfoot deformity. Diagnosis The diagnosis of tibialis posterior dysfunction is essentially clinical. However, plain radiographs of the foot and ankle are useful for assessing the degree of deformity and to confirm the presence or absence of degenerative changes in the subtalar and ankle articulations. The radiographs are also useful to exclude other causes of an acquired flatfoot deformity. The most useful radiographs are bilateral anteroposterior and lateral radiographs of the foot and a mortise (true anteroposterior) view of the ankle. All radiographs should be done with the patient standing. In most cases we see no role for magnetic resonance imaging or ultrasonography, as the diagnosis can be made clinically. Non surgical Treatment Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In many cases of PTTD, treatment can begin with non-surgical approaches that may include. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe. Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weight-bearing for a while. Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may advise changes to make with your shoes and may provide special inserts designed to improve arch support.  Surgical Treatment The indications for surgery are persistent pain and/or significant deformity. Sometimes the foot just feels weak and the assessment of deformity is best done by a foot and ankle specialist. If surgery is appropriate, a combination of soft tissue and bony procedures may be considered to correct alignment and support the medial arch, taking strain off failing ligaments. Depending upon the tissues involved and extent of deformity, the foot and ankle specialist will determine the necessary combination of procedures. Surgical procedures may include a medial slide calcaneal osteotomy to correct position of the heel, a lateral column lengthening to correct position in the midfoot and a medial cuneiform osteotomy or first metatarsal-tarsal fusion to correct elevation of the medial forefoot. The posterior tibial tendon may be reconstructed with a tendon transfer. In severe cases (stage III), the reconstruction may include fusion of the hind foot,, resulting in stiffness of the hind foot but the desired pain relief. In the most severe stage (stage IV), the deltoid ligament on the inside of the ankle fails, resulting in the deformity in the ankle. This deformity over time can result in arthritis in the ankle.
Surgical Treatment The indications for surgery are persistent pain and/or significant deformity. Sometimes the foot just feels weak and the assessment of deformity is best done by a foot and ankle specialist. If surgery is appropriate, a combination of soft tissue and bony procedures may be considered to correct alignment and support the medial arch, taking strain off failing ligaments. Depending upon the tissues involved and extent of deformity, the foot and ankle specialist will determine the necessary combination of procedures. Surgical procedures may include a medial slide calcaneal osteotomy to correct position of the heel, a lateral column lengthening to correct position in the midfoot and a medial cuneiform osteotomy or first metatarsal-tarsal fusion to correct elevation of the medial forefoot. The posterior tibial tendon may be reconstructed with a tendon transfer. In severe cases (stage III), the reconstruction may include fusion of the hind foot,, resulting in stiffness of the hind foot but the desired pain relief. In the most severe stage (stage IV), the deltoid ligament on the inside of the ankle fails, resulting in the deformity in the ankle. This deformity over time can result in arthritis in the ankle.